N18.1-5/N18.9
CAUTION
Check all medicines for possible dose adjustment based on eGFR/CrCl.
The doses of many medicines need to be adjusted in renal impairment. Recommendations for medicines that require dose adjustment in renal impairment can be found in the SAMF, package insert, and from many online resources e.g.: http://www.globalrph.com/index_renal.htm
DESCRIPTION
Structural or functional kidney damage present for > 3 months, with or without a decreased glomerular filtration rate (eGFR).
Markers of kidney damage include:
- abnormalities in urine e.g. proteinuria or haematuria
- abnormalities in blood e.g. serum creatinine or low eGFR
- abnormalities in imaging tests e.g. small kidneys on ultrasound
- abnormalities on pathological specimens e.g. glomerular disease on renal biopsy
Common causes of chronic kidney disease include:
- hypertension
- diabetes mellitus
- glomerular diseases
- polycystic kidney disease
- HIV/AIDS
Chronic kidney disease can be entirely asymptomatic, BUT early detection and management can improve the outcome of this condition.
Treatment and prevention strategies according to prognostic category
Estimation of the degree of kidney damage is important to guide management to prevent adverse outcomes of chronic kidney disease.
Use eGFR and albumin creatinine ratio to put patient into prognostic category- see table below.
Note:
- Adults with mild to moderate decline in eGFR and no albuminuria can all be managed at primary care level once the cause and plan for care has been established.
- All children should be referred for investigation and initial management.
Prognosis of CKD by GFR and albuminuria categories: KDIGO 2012
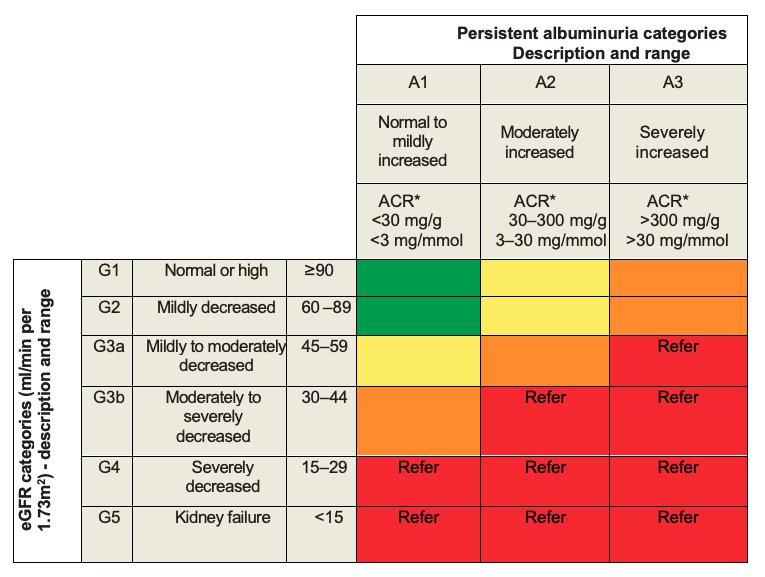
*ACR: albumin to creatinine ratio in urine specimen.
Green: low risk (if no other markers of kidney disease, no CKD); yellow: moderately increased risk; orange: high risk; red: very high risk; A1, A2, A3 = categories of albuminuria; G1, G2, G3a, G3b, G4, G5 = categories of eGFR
Adapted from: Levin A, Stevens PE. Summary of KDIGO 2012 CKD Guideline: behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 2014 Jan;85(1):49-61. https://www.ncbi.nlm.nih.gov/pubmed/24284513
Send blood annually for measurement of creatinine in all patients at increased risk. (eGFR will be calculated by the laboratory, based on the serum creatinine).
GENERAL MEASURES
- Reduce salt intake.
- Low protein diet is indicated in the presence of CKD stage 4 and 5.
- Reduce cardiovascular disease risk factors. See Prevention of ischaemic heart disease and atherosclerosis
- Avoid nephrotoxic drugs e.g. NSAIDs, tenofovir.
- Screen for proteinuria.
- If urine dipstick 1+ or greater, repeat on a properly collected midstream urine specimen on another occasion. If proteinuria persists quantify protein with a spot urine protein creatinine ratio. Significant proteinuria = spot urine protein creatinine ratio of > 0.1 g/mmol. This is equivalent to 1g per 24 hours.
- Note: Proteinuria is screened for differently in diabetics. See Diabetic nephropathy
MEDICINE TREATMENT
Treat underlying conditions.
Proteinuria
Measure serum potassium at baseline.
Adults
- ACE-inhibitor, e.g.:
- Enalapril, oral, start with 5 mg 12 hourly.
- Titrate up to 10 mg 12 hourly, if tolerated.
- Start with low dosage of ACE-inhibitor and titrate up to the maximum dose or until the proteinuria disappears - whichever comes first. Ensure BP remains in normal range and no side effects are present.
- Monitor creatinine and potassium:
- 1–2 weeks after treatment initiation, if eGFR < 60 mL/min and after 4 weeks, if eGFR > 60 mL/min.
- If creatinine increases by > 20% from the baseline, stop ACE-inhibitor and refer.
- If stable, monitor thereafter at regular clinic visits.
- ACE-inhibitors are contraindicated in, amongst others:
- hyperkalaemia
- known hypersensitivity to an ACE-inhibitor or an ARB
- bilateral renal artery stenosis
- pregnancy
- severe renal impairment (eGFR < 30 mL/min)
Hyperlipidaemia
If hyperlipidaemia is a co-existent risk factor, manage according to Prevention of ischaemic heart disease and atherosclerosis
Diabetes mellitus
- In diabetics, optimise control according to Diabetes mellitus type 2, in adults
- Replace oral sulphonylureas with insulin when eGFR < 60 mL/min, because of an increased risk of hypoglycaemia.
- Replace metformin with insulin when eGFR < 30 mL/min, because of the potential risk of lactic acidosis.
- Insulin is preferred to control blood glucose in patients with eGFR < 30 mL/min.
Hypertension
Treat if present. See Hypertension
Fluid overload
Treat fluid overload if present and refer.
Adults
- Furosemide, slow IV or oral, 40–80 mg, 12 hourly.
- If poor response, repeat after 1 hour.
- Do not give IV fluids - use heparin lock or similar IV access.
Children
- Furosemide, IV, 1 mg/kg, over 5 minutes. See paediatric dosing table.
- Do not put up a drip or run in any IV fluids.
Note: Exclude heart failure in patients with persistent pedal oedema.
REFERRAL
- All cases of suspected chronic kidney disease stages 3–5 for assessment and planning.
- All children.
- All cases of CKD with:
- haematuria,
- significant proteinuria with urine protein creatinine ratio of > 0.1 g/mmol
- eGFR < 60 mL/min for initial assessment and planning
- eGFR < 30 mL/min
- Uncontrolled hypertension/fluid overload.
- CKD associated with hyperlipidaemia.
- No reduction of proteinuria with ACE-inhibitor therapy.
- If ACE-inhibitors are contra-indicated.
- If ACE-inhibitors are not tolerated.
Patients who might qualify for dialysis and transplantation or who have complications should be referred early to ensure improved outcome and survival on dialysis, i.e. as soon as eGFR drops < 30 mL/min, or as soon as diagnosis is made/suspected.