A98.0/A98.1/A98.2/A98.3/A98.4/A98.4/A98.5/A98.8/A99/A91
Note: notifiable medical conditions.
Consult the most recent Viral Haemorrhagic Fever Guidelines from the National Department of Health.
DESCRIPTION
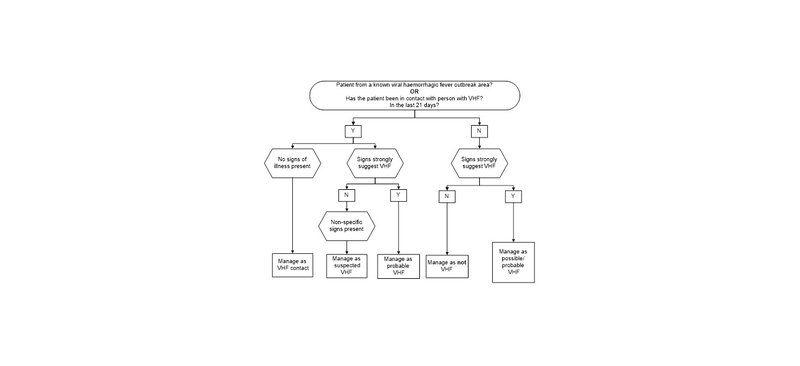
Viral haemorrhagic fevers (VHF) are uncommon conditions in South Africa. They may present with non-specific signs (fever, headache, conjunctivitis, pharyngitis, myalgia (especially lower back pain), diarrhea, vomiting, abdominal pain) or with signs strongly suggestive of VHF (petechial rash, ecchymoses, other haemorrhagic signs e.g. epistaxis, haematemesis and melaena). Other symptoms and organ involvement may be variable.
More than 90% of suspected cases of VHF in South Africa prove to be severe forms of common diseases. Many of the diseases mistaken for VHF are treatable if diagnosed early.
These include:
- Severe tick bite fever.
- Fulminant hepatitis.
- Severe falciparum malaria.
- Leptospirosis.
- Severe bacterial infections, particularly N. meningitidis.
Endemic causes of VHF in South Africa are Crimean-Congo fever and Rift Valley Fever, both of which may be transmitted between humans by means of blood and body fluids. Imported conditions include Lassa, Ebola and Marburg Fever amongst others.
Obtaining a history of possible exposure to infection (including a detailed travel history) is crucial to diagnosing VHF. Relatives and friends often provide more reliable information than severely ill patients.
GENERAL MEASURES
All suspected, probable VHF cases and contacts of VHF cases must be discussed and managed in consultation with the Regional Virologist or Infectious Diseases Consultant at the referral centre.
Cases should also be discussed with the Special Pathogens Unit of the National Institute for Communicable Diseases (NICD):
Tel: 011 386 6000, Outbreak hotline: 082 883 9920
Transfer of patients will only occur once all relevant arrangements have been made to limit further exposure to a potentially contagious and life threatening agent.
Viral haemorrhagic fevers (VHF) are readily transmitted to healthcare workers, so it is essential to apply strict contact precautions.
ISOLATE ALL SUSPECTED SYMPTOMATIC CASES AT ALL TIMES
If VHF is considered, isolate patient in a single room and take proper precautions to limit further exposure. These include where available:
- long sleeved disposable gown,
- waterproof apron if the patient is bleeding,
- two pairs of latex gloves, one underneath the gown and one with the wrist of the glove pulled over the gown wrist
- disposable face mask (preferably with a visor),
- goggles if a mask without the visor is used,
- waterproof boots or 2 pairs of overshoes, one over the other.
Note: Do not touch your own skin with your gloved hands.
MANAGEMENT
| Signs strongly suggesting VHF | Non-specific signs that may occur with VHF |
|
|
|
Management of VHF contact
- Consult clinician, discuss with NICD and isolate patient (See above).
- Record and follow up all patient contacts.
Management of suspected/possible/probable VHF
- Non-specific signs:
- Consult with clinician, discuss with NICD, isolate patient, initiate ceftriaxone and record and follow-up all patient contacts.
- Signs strongly suggestive of VHF:
- Consult with a clinician, discuss with NICD, isolate patient, initiate ceftriaxone and arrange transfer with EMS (providing patient’s VHF status, and names, addresses and telephone numbers of patient contacts).
Adults
- Ceftriaxone, IV, 2 g immediately.
Children
- Ceftriaxone, IM, 80 mg/kg/dose immediately as a single dose. See paediatric dosing tool.
- Do not inject more than 1 g at one injection site.
CAUTION: USE OF CEFTRIAXONE IN NEONATES AND CHILDREN
- If SUSPECTING SERIOUS BACTERIAL INFECTION in neonate, give ceftriaxone, even if jaundiced.
- Avoid giving calcium-containing IV fluids (e.g. Ringer Lactate) together with ceftriaxone:
- If ≤ 28 days old, avoid calcium-containing IV fluids for 48 hours after ceftriaxone administered.
- If > 28 days old, ceftriaxone and calcium-containing IV fluids may be given sequentially provided the giving set is flushed thoroughly with sodium chloride 0.9% before and after.
- Preferably administer IV fluids without calcium contents.
- Always include the dose and route of administration of ceftriaxone in the referral letter.
REFERRAL
- All cases, after consultation with clinician, discussion with NICD, isolation of patient and management of acute condition.
Manage all contacts of VHF cases according to the current national guidelines. Ensure that contact details are obtained and that there is a plan to manage contacts.